Introduction
Radiography is a cornerstone of modern medical diagnosis, providing critical insights into internal structures and pathologies. However, the diagnostic value of any radiographic image depends heavily on proper exposure techniques. Underexposed X-rays—those lacking sufficient radiation energy—present as overly light images with diminished detail, potentially compromising patient care. This guide explores the technical aspects of underexposure, its clinical implications, and evidence-based strategies for consistently producing diagnostic-quality radiographs while maintaining radiation safety standards.
What Defines an Underexposed Radiograph?
Underexposure in radiography occurs when insufficient X-ray energy penetrates the anatomical structures being imaged. These suboptimal exposures manifest with distinct characteristics:
– Excessively light or white appearance across the image
– Reduced contrast between different tissue densities
– Elevated quantum noise (visible as graininess or speckled appearance in the image)
– Poor visualization of crucial anatomical structures
– Diminished diagnostic value requiring potential repeat exposures
Radiologists and technologists recognize underexposed images by their lack of optical density (darkness level in the image) and insufficient contrast resolution (ability to distinguish between similar tissues), making subtle pathologies particularly difficult to detect.
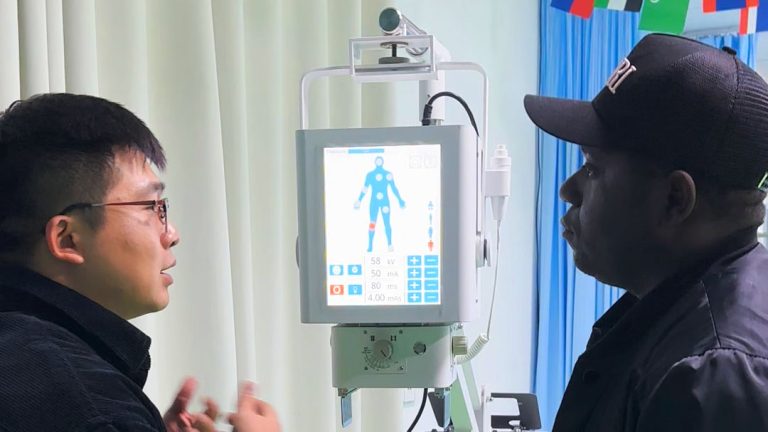
Technical Causes of Radiographic Underexposure
Understanding the technical parameters that influence exposure is essential for preventing diagnostic errors. Underexposure typically results from:
Inappropriate Technical Factors:
– Insufficient kilovoltage peak (kVp) settings, reducing beam penetration. Think of kVp as the “quality” of the X-ray beam—like voltage in electronics—determining how deeply X-rays penetrate tissue.
– Inadequate milliampere-seconds (mAs) values, limiting photon production. Consider mAs as the “quantity” of the X-ray beam—similar to current in electronics—controlling how many X-ray photons are produced.
– Incorrect exposure time selections, particularly for moving structures
Equipment and Procedural Issues:
– X-ray generator malfunction or calibration errors
– Improper grid ratio selection or positioning (grids are devices that improve image quality by removing scattered radiation, much like how polarized sunglasses reduce glare)
– Automatic Exposure Control (AEC) sensor misalignment or malfunction (AEC works similarly to the automatic exposure feature on a camera)
– Excessive source-to-image distance (SID) without compensatory adjustments (the distance between the X-ray tube and the image receptor, which affects image intensity like moving a flashlight further from an object)
Patient-Specific Factors:
– Inaccurate patient positioning altering tissue density presentation
– Failure to adjust technical factors for patient size, age, or condition
– Inadequate compression of compressible anatomical regions (compression works like squeezing a thick book to make it easier to see through)
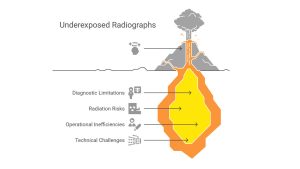
Clinical Impact of Underexposed Radiographs
The consequences of underexposure extend beyond image quality concerns, affecting multiple aspects of patient care:
Diagnostic Limitations:
– Missed or delayed detection of subtle pathologies
– Incorrect interpretation of anatomical relationships
– Inadequate visualization of critical diagnostic features
Radiation Protection Concerns:
– Increased cumulative radiation dose from necessary repeat exposures
– Additional radiation exposure for vulnerable patient populations
– Occupational exposure risks for radiography staff
Operational Efficiency:
– Extended examination times for repeated procedures
– Delayed diagnosis and treatment planning
– Increased resource utilization and departmental costs
– Reduced patient throughput in imaging departments
Evidence-Based Prevention Strategies
Implementing systematic approaches to exposure optimization ensures consistent, diagnostic-quality images:
Technical Protocol Implementation:
– Develop and adhere to evidence-based radiographic technique charts
– Implement standardized positioning guides for common examinations
– Establish quality control procedures for exposure parameter verification
Digital Radiography Optimization:
– Utilize exposure index monitoring for immediate feedback on technique appropriateness (similar to how a light meter works in photography)
– Implement post-processing algorithms designed to compensate for minor exposure variations
– Conduct regular calibration of digital detector systems
Professional Development:
– Provide ongoing education for radiographers on exposure principles
– Ensure comprehensive training on equipment-specific features
– Implement peer review processes for radiographic technique evaluation
Quality Assurance Programs:
– Establish departmental rejection analysis systems to identify exposure trends
– Conduct regular equipment performance evaluations
– Implement continuous improvement processes based on exposure data analysis
Conclusion
Radiographic underexposure represents a significant challenge in diagnostic imaging that impacts patient care, radiation safety, and operational efficiency. By understanding the technical factors contributing to underexposure and implementing systematic prevention strategies, imaging professionals can consistently produce diagnostic-quality radiographs while minimizing radiation exposure. This commitment to technical excellence ensures that radiography continues to serve as a valuable, safe, and efficient diagnostic tool in modern healthcare.
Frequently Asked Questions
1) How can I quickly identify an underexposed radiograph?
Underexposed radiographs appear noticeably lighter than properly exposed images, with reduced contrast between structures and increased graininess or noise. Critical anatomical details may be difficult to visualize, particularly in regions with similar tissue densities.
2) What immediate actions should be taken when underexposure is identified?
When underexposure is detected, evaluate the technical factors used, check equipment function, and review positioning techniques before considering a repeat exposure. For digital systems, assess whether post-processing adjustments might enhance the existing image before resorting to additional radiation exposure.
3) How do digital and conventional radiography differ in managing underexposure?
Digital radiography offers a wider dynamic range and post-processing capabilities that can partially compensate for minor exposure errors. However, severely underexposed digital images still suffer from excessive quantum noise that cannot be eliminated through processing alone. Conventional film-screen systems have a narrower exposure latitude (like traditional photography film with less forgiveness for exposure errors), making proper technical selection even more critical.
4) What role does continuing education play in preventing underexposure?
Ongoing professional development ensures radiographers maintain current knowledge of exposure principles, equipment capabilities, and patient-specific adaptations. Regular training reduces technical errors and promotes consistent application of evidence-based exposure protocols across diverse clinical scenarios.